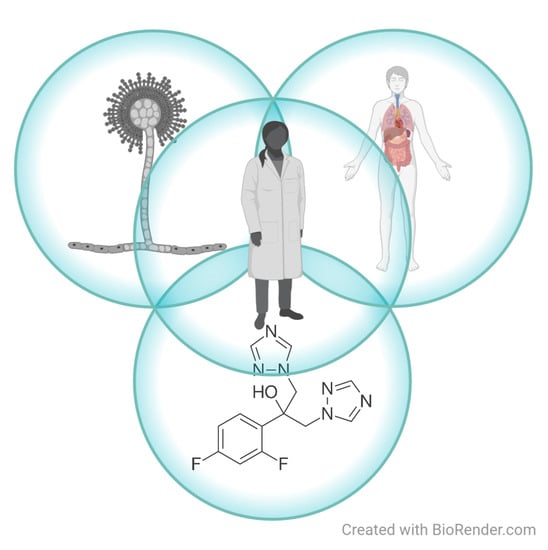
The Multifaceted Role of Mating Type of the Fungus and Sex of the Host in Studies of Fungal Infections in Humans
Abstract
:1. Introduction
2. Sex of the Fungi That Cause Infections
2.1. Aspergillus Diseases and Reproduction of the Fungus Aspergillus fumigatus
2.2. Cryptococcal Diseases and Reproduction of the Fungus Cryptococcus neoformans
2.3. Candida Infection and Reproduction of Candida albicans
3. Difference of Sex and Gender of the Human Host in Susceptibility to Fungal Infection
3.1. Is Awareness of Invasive Fungal Diseases Independent of Gender?
3.2. Who Can Get a Fungal Infection?
3.3. Is There a Sex-Dependent Difference in the Human Immune Response?
3.4. Susceptibility to Infection with the Fungus Aspergillus fumigatus by Sex/Gender
3.5. Susceptibility to Infection with the Fungus Cryprococcus neoformans by Sex/Gender
3.6. Susceptibility to Infection with the Fungus Paracoccidioides brasiliensis Is Sex/Gender Dependent
3.7. Incidence of Dermatophytosis Associated with Differences in Lifestyle between Women and Men
3.8. Incidence of Candidiasis in Relation to Life Circumstances
4. The Impact of the Sex of Participants in an Antifungal Trial
How Can Sex Differences Be More Clearly Highlighted in Cell-Based Studies and Later Preclinical and Clinical Studies?
5. Antifungals and Fungicides and Known Resistance Mechanisms
5.1. Posaconazole Is Well Tolerated Regardless of Age, Sex, Race, or Ethnicity
5.2. Fluconazole Stimulates Fungi to Reproduce Sexually
5.3. Retinoids in Fungal Infections
6. Conclusions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Meyer, V.; Andersen, M.R.; Brakhage, A.A.; Braus, G.H.; Caddick, M.X.; Cairns, T.C.; de Vries, R.P.; Haarmann, T.; Hansen, K.; Hertz-Fowler, C.; et al. Current challenges of research on filamentous fungi in relation to human welfare and a sustainable bio-economy: A white paper. Fungal Biol. Biotechnol. 2016, 3, 6. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meyer, V.; Basenko, E.Y.; Benz, J.P.; Braus, G.H.; Caddick, M.X.; Csukai, M.; de Vries, R.P.; Endy, D.; Frisvad, J.C.; Gunde-Cimerman, N.; et al. Growing a circular economy with fungal biotechnology: A white paper. Fungal Biol. Biotechnol. 2020, 7, 5. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Butler, G. Fungal Sex and Pathogenesis. Clin. Microbiol. Rev. 2010, 23, 140–159. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kohler, J.R.; Casadevall, A.; Perfect, J. The Spectrum of Fungi That Infects Humans. Cold Spring Harb. Perspect. Med. 2015, 5, a019273. [Google Scholar] [CrossRef] [Green Version]
- Westman, J.; Hube, B.; Fairn, G.D. Integrity under stress: Host membrane remodelling and damage by fungal pathogens. Cell. Microbiol. 2019, 21, e13016. [Google Scholar] [CrossRef] [Green Version]
- Drott, M.T. Sex and self defense. Elife 2021, 10, e73723. [Google Scholar] [CrossRef]
- The Annual Event of the Commission for Equal Opportunities in Science: The Ovelooked Dimensions of Gender in Scientific Research. Available online: https://www.gov.si/dogodki/2020-03-09-posvet-komisije-za-enake-moznosti-na-podrocju-znanosti/ (accessed on 7 April 2022).
- Galea, L.A.M.; Choleris, E.; Albert, A.Y.K.; McCarthy, M.M.; Sohrabji, F. The promises and pitfalls of sex difference research. Front. Neuroendocrinol. 2020, 56, 100817. [Google Scholar] [CrossRef]
- Tannenbaum, C.; Ellis, R.P.; Eyssel, F.; Zou, J.; Schiebinger, L. Sex and gender analysis improves science and engineering. Nature 2019, 575, 137–146. [Google Scholar] [CrossRef] [Green Version]
- Plotina Project: ReGendering Science—For an Inclusive Research Environment. Incorporating Gender Variables or Gender in Research. Available online: https://www.plotina.eu/plotina-final-conference/ (accessed on 7 April 2022).
- Ene, I.V.; Bennett, R.J. The cryptic sexual strategies of human fungal pathogens. Nat. Rev. Microbiol. 2014, 12, 239–251. [Google Scholar] [CrossRef] [Green Version]
- Heitman, J.; Carter, D.A.; Dyer, P.S.; Soll, D.R. Sexual Reproduction of Human Fungal Pathogens. Cold Spring Harb. Perspect. Med. 2014, 4, a019281. [Google Scholar] [CrossRef] [Green Version]
- Heitman, J.; Sun, S.; James, T.Y. Evolution of fungal sexual reproduction. Mycologia 2013, 105, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Latgé, J.-P. Aspergillus fumigatus and Aspergillosis. Clin. Microbiol. Rev. 1999, 12, 310–350. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Latgé, J.-P. The pathobiology of Aspergillus fumigatus. Trends Microbiol. 2001, 9, 382–389. [Google Scholar] [CrossRef]
- Brakhage, A.A.; Langfelder, K. Menacing Mold: The Molecular Biology of Aspergillus fumigatus. Annu. Rev. Microbiol. 2002, 56, 433–455. [Google Scholar] [CrossRef] [PubMed]
- Dagenais, T.R.T.; Keller, N.P. Pathogenesis of Aspergillus fumigatus in Invasive Aspergillosis. Clin. Microbiol. Rev. 2009, 22, 447–465. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tekaia, F.; Latgé, J.-P. Aspergillus fumigatus: Saprophyte or pathogen? Curr. Opin. Microbiol. 2005, 8, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Hohl, T.M.; Feldmesser, M. Aspergillus fumigatus: Principles of Pathogenesis and Host Defense. Eukaryot. Cell 2007, 6, 1953–1963. [Google Scholar] [CrossRef] [Green Version]
- Abad, A.; Victoria Fernández-Molina, J.; Bikandi, J.; Ramírez, A.; Margareto, J.; Sendino, J.; Luis Hernando, F.; Pontón, J.; Garaizar, J.; Rementeria, A. What makes Aspergillus fumigatus a successful pathogen? Genes and molecules involved in invasive aspergillosis. Rev. Iberoam. Micol. 2010, 27, 155–182. [Google Scholar] [CrossRef]
- Kwon-Chung, K.J.; Sugui, J.A. Aspergillus fumigatus—What Makes the Species a Ubiquitous Human Fungal Pathogen? PLoS Pathog. 2013, 9, e1003743. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/fungal/diseases/index.html (accessed on 19 December 2019).
- Losada, L.; Sugui, J.A.; Eckhaus, M.A.; Chang, Y.C.; Mounaud, S.; Figat, A.; Joardar, V.; Pakala, S.B.; Pakala, S.; Venepally, P.; et al. Genetic Analysis Using an Isogenic Mating Pair of Aspergillus fumigatus Identifies Azole Resistance Genes and Lack of MAT Locus’s Role in Virulence. PLoS Pathog. 2015, 11, e1004834. [Google Scholar] [CrossRef]
- Rhodes, J.; Fisher, M.C. Global epidemiology of emerging Candida auris. Curr. Opin. Microbiol. 2019, 52, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Jackson, B.R.; Chow, N.; Forsberg, K.; Litvintseva, A.P.; Lockhart, S.R.; Welsh, R.; Vallabhaneni, S.; Chiller, T. On the Origins of a Species: What Might Explain the Rise of Candida auris? J. Fungi 2019, 5, 58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ross, Z.K.; Lorenz, A. Is Candida auris sexual? PLoS Pathog. 2020, 16, e1009094. [Google Scholar] [CrossRef]
- Muñoz, J.F.; Gade, L.; Chow, N.A.; Loparev, V.N.; Juieng, P.; Berkow, E.L.; Farrer, R.A.; Litvintseva, A.P.; Cuomo, C.A. Genomic insights into multidrug-resistance, mating and virulence in Candida auris and related emerging species. Nat. Commun. 2018, 9, 5346. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deegan, D.F.; Engel, N. Sexual Dimorphism in the Age of Genomics: How, When, Where. Front. Cell Dev. Biol. 2019, 7, 186. [Google Scholar] [CrossRef] [PubMed]
- Boerner, K.E.; Chambers, C.T.; Gahagan, J.; Keogh, E.; Fillingim, R.B.; Mogil, J.S. Conceptual complexity of gender and its relevance to pain. Pain 2018, 159, 2137–2141. [Google Scholar] [CrossRef]
- Lee, S.K. Sex as an important biological variable in biomedical research. BMB Rep. 2018, 51, 167–173. [Google Scholar] [CrossRef] [Green Version]
- Benedict, K.; Molinari, N.A.M.; Jackson, B.R. Public Awareness of Invasive Fungal Diseases—United States, 2019. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1343–1346. [Google Scholar] [CrossRef]
- Seagle, E.E.; Williams, S.L.; Chiller, T.M. Recent Trends in the Epidemiology of Fungal Infections. Infect. Dis. Clin. N. Am. 2021, 35, 237–260. [Google Scholar] [CrossRef]
- Köhler, J.R.; Hube, B.; Puccia, R.; Casadevall, A.; Perfect, J.R. Fungi that Infect Humans. Microbiol. Spectr. 2017, 5, 813–843. [Google Scholar] [CrossRef]
- Friedman, D.Z.; Schwartz, I.S. Emerging Fungal Infections: New Patients, New Patterns, and New Pathogens. J. Fungi 2019, 5, 67. [Google Scholar] [CrossRef] [Green Version]
- Klein, S.L.; Flanagan, K.L. Sex differences in immune responses. Nat. Rev. Immunol. 2016, 16, 626–638. [Google Scholar] [CrossRef]
- Alvergne, A.; Högqvist Tabor, V. Is Female Health Cyclical? Evolutionary Perspectives on Menstruation. Trends Ecol. Evol. 2018, 33, 399–414. [Google Scholar] [CrossRef] [Green Version]
- Giefing-Kröll, C.; Berger, P.; Lepperdinger, G.; Grubeck-Loebenstein, B. How sex and age affect immune responses, susceptibility to infections, and response to vaccination. Aging Cell 2015, 14, 309–321. [Google Scholar] [CrossRef]
- vom Steeg, L.G.; Klein, S.L. SeXX Matters in Infectious Disease Pathogenesis. PLoS Pathog. 2016, 12, e1005374. [Google Scholar] [CrossRef] [Green Version]
- Gay, L.; Melenotte, C.; Lakbar, I.; Mezouar, S.; Devaux, C.; Raoult, D.; Bendiane, M.-K.; Leone, M.; Mège, J.-L. Sexual Dimorphism and Gender in Infectious Diseases. Front. Immunol. 2021, 12, 698121. [Google Scholar] [CrossRef]
- Silveyra, P.; Fuentes, N.; Rodriguez Bauza, D.E. Sex and Gender Differences in Lung Disease. In Lung Inflammation in Health and Disease; Springer: Cham, Switzerland, 2021; Volume II, pp. 227–258. [Google Scholar]
- Sun, K.-S.; Tsai, C.-F.; Chen, S.C.-C.; Chen, Y.-Y.; Huang, W.-C. Galactomannan Testing and the Incidence of Invasive Pulmonary Aspergillosis: A 10-Year Nationwide Population-Based Study in Taiwan. PLoS ONE 2016, 11, e0149964. [Google Scholar] [CrossRef]
- Apostolopoulou, A.; Esquer Garrigos, Z.; Vijayvargiya, P.; Lerner, A.H.; Farmakiotis, D. Invasive Pulmonary Aspergillosis in Patients with SARS-CoV-2 Infection: A Systematic Review of the Literature. Diagnostics 2020, 10, 807. [Google Scholar] [CrossRef]
- Dellière, S.; Dudoignon, E.; Fodil, S.; Voicu, S.; Collet, M.; Oillic, P.-A.; Salmona, M.; Dépret, F.; Ghelfenstein-Ferreira, T.; Plaud, B.; et al. Risk factors associated with COVID-19-associated pulmonary aspergillosis in ICU patients: A French multicentric retrospective cohort. Clin. Microbiol. Infect. 2021, 27, 790.e1–790.e5. [Google Scholar] [CrossRef]
- Duan, Y.; Ou, X.; Chen, Y.; Liang, B.; Ou, X. Severe Influenza With Invasive Pulmonary Aspergillosis in Immunocompetent Hosts: A Retrospective Cohort Study. Front. Med. 2021, 7, 1115. [Google Scholar] [CrossRef]
- Jhun, B.W.; Jung, W.J.; Hwang, N.Y.; Park, H.Y.; Jeon, K.; Kang, E.-S.; Koh, W.-J. Risk factors for the development of chronic pulmonary aspergillosis in patients with nontuberculous mycobacterial lung disease. PLoS ONE 2017, 12, e0188716. [Google Scholar] [CrossRef]
- Jain, A.K.; Puri, M.; Tayal, D.; Singhal, R.; Sarin, R. Prevalence of allergic bronchopulmonary aspergillosis in asthmatic patients: A prospective institutional study. Indian J. Tuberc. 2018, 65, 285–289. [Google Scholar] [CrossRef]
- Grehn, C.; Eschenhagen, P.; Temming, S.; Düesberg, U.; Neumann, K.; Schwarz, C. Urban Life as Risk Factor for Aspergillosis. Front. Cell. Infect. Microbiol. 2020, 10, 681. [Google Scholar] [CrossRef]
- Thomas, A.; Jackson, D.J.; Tisler, C.J.; Rajamanickam, V.; Gangnon, R.E.; Lemanske, R.F. Sex-related Differences in Atopic Phenotype Expression and Immune Responses in Childhood. J. Allergy Clin. Immunol. 2012, 129, AB6. [Google Scholar] [CrossRef]
- Guess, T.; Rosen, J.; McClelland, E. An Overview of Sex Bias in C. neoformans Infections. J. Fungi 2018, 4, 49. [Google Scholar] [CrossRef] [Green Version]
- Casadevall, A.; Perfect, J.R. Cryptococcus Neoformans; ASM Press: Washington, DC, USA, 1998; Volume 595. [Google Scholar]
- van den Berg, M.C.W.; Woerlee, J.Z.; Ma, H.; May, R.C. Sex-Dependent Resistance to the Pathogenic Fungus Cryptococcus neoformans. Genetics 2006, 173, 677–683. [Google Scholar] [CrossRef] [Green Version]
- Bellissimo-Rodrigues, F.; Bollela, V.R.; Da Fonseca, B.A.L.; Martinez, R. Endemic paracoccidioidomycosis: Relationship between clinical presentation and patients’ demographic features. Med. Mycol. 2013, 51, 313–318. [Google Scholar] [CrossRef] [Green Version]
- Restrepo, A.; Gómez, B.L.; Tobón, A. Paracoccidioidomycosis: Latin America’s Own Fungal Disorder. Curr. Fungal Infect. Rep. 2012, 6, 303–311. [Google Scholar] [CrossRef]
- Bernin, H.; Lotter, H. Sex Bias in the Outcome of Human Tropical Infectious Diseases: Influence of Steroid Hormones. J. Infect. Dis. 2014, 209, S107–S113. [Google Scholar] [CrossRef] [Green Version]
- Blotta, M.H.; Mamoni, R.L.; Oliveira, S.J.; Nouer, S.A.; Papaiordanou, P.M.; Goveia, A.; Camargo, Z.P.D. Endemic regions of paracoccidioidomycosis in Brazil: A clinical and epidemiologic study of 584 cases in the southeast region. The American journal of tropical medicine and hygiene. Am. J. Trop. Med. Hyg. 1999, 61, 390–394. [Google Scholar] [CrossRef]
- de Castro, L.F.; Ferreira, M.C.; da Silva, R.M.; de Souza Lima Blotta, M.H.; Longhi, L.N.A.; Mamoni, R.L. Characterization of the immune response in human paracoccidioidomycosis. J. Infect. 2013, 67, 470–485. [Google Scholar] [CrossRef]
- Pinzan, C.F.; Ruas, L.P.; Casabona-Fortunato, A.S.; Carvalho, F.C.; Roque-Barreira, M.-C. Immunological Basis for the Gender Differences in Murine Paracoccidioides brasiliensis Infection. PLoS ONE 2010, 5, e10757. [Google Scholar] [CrossRef] [Green Version]
- Shemer, A.; Babaev, M. Fungal Infections (Onychomycosis, Tinea Pedis, Tinea Cruris, Tinea Capitis, Tinea Manuum, Tinea Corporis, different Candida Infections, and Pityriasis Versicolor) and Mycological Laboratory Analyses. In Gender and Dermatology; Springer International Publishing: Cham, Switzerland, 2018; pp. 235–242. [Google Scholar]
- Rosen, T. Evaluation of gender as a clinically relevant outcome variable in the treatment of onychomycosis with efinaconazole topical solution 10. Cutis 2015, 96, 197–201. [Google Scholar]
- D’enfert, C.; Kaune, A.-K.; Alaban, L.-R.; Chakraborty, S.; Cole, N.; Delavy, M.; Kosmala, D.; Marsaux, B.; Fróis-Martins, R.; Morelli, M.; et al. The impact of the Fungus-Host-Microbiota interplay upon Candida albicans infections: Current knowledge and new perspectives. FEMS Microbiol. Rev. 2021, 45, fuaa060. [Google Scholar] [CrossRef]
- Sobel, J.D. Vulvovaginal candidosis. Lancet 2007, 369, 1961–1971. [Google Scholar] [CrossRef]
- Foxman, B.; Muraglia, R.; Dietz, J.-P.; Sobel, J.D.; Wagner, J. Prevalence of Recurrent Vulvovaginal Candidiasis in 5 European Countries and the United States. J. Low. Genit. Tract. Dis. 2013, 17, 340–345. [Google Scholar] [CrossRef]
- Gajer, P.; Brotman, R.M.; Bai, G.; Sakamoto, J.; Schütte, U.M.E.; Zhong, X.; Koenig, S.S.K.; Fu, L.; Ma, Z.; Zhou, X.; et al. Temporal Dynamics of the Human Vaginal Microbiota. Sci. Transl. Med. 2012, 4, 132ra52. [Google Scholar] [CrossRef] [Green Version]
- Ferwerda, B.; Ferwerda, G.; Plantinga, T.S.; Willment, J.A.; van Spriel, A.B.; Venselaar, H.; Elbers, C.C.; Johnson, M.D.; Cambi, A.; Huysamen, C.; et al. Human Dectin-1 Deficiency and Mucocutaneous Fungal Infections. N. Engl. J. Med. 2009, 361, 1760–1767. [Google Scholar] [CrossRef] [Green Version]
- He, Y.; Tang, R.; Deng, J.; Cai, T.; He, P.; Wu, J.; Cao, Y. Effects of oestrogen on vulvovaginal candidosis. Mycoses 2021, 65, 4–12. [Google Scholar] [CrossRef]
- Al-Janabi, A.A.H.S.; Jawad, R.K.M. Estrogen on Candida spp. of the Vagina: Is there any effect? Int. J. Med. Rev. 2021, 8, 134–139. [Google Scholar]
- Mauvais-Jarvis, F.; Bairey Merz, N.; Barnes, P.J.; Brinton, R.D.; Carrero, J.-J.; DeMeo, D.L.; De Vries, G.J.; Epperson, C.N.; Govindan, R.; Klein, S.L.; et al. Sex and gender: Modifiers of health, disease, and medicine. Lancet 2020, 396, 565–582. [Google Scholar] [CrossRef]
- Ingersoll, M.A. Sex differences shape the response to infectious diseases. PLoS Pathog. 2017, 13, e1006688. [Google Scholar] [CrossRef] [PubMed]
- Heidari, S.; Babor, T.F.; De Castro, P.; Tort, S.; Curno, M. Sex and Gender Equity in Research: Rationale for the SAGER guidelines and recommended use. Res. Integr. Peer Rev. 2016, 1, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kim, J.Y.; Min, K.; Paik, H.Y.; Lee, S.K. Sex omission and male bias are still widespread in cell experiments. Am. J. Physiol. Cell Physiol. 2021, 320, C742–C749. [Google Scholar] [CrossRef]
- Park, M.-N.; Park, J.H.; Paik, H.Y.; Lee, S.K. Insufficient sex description of cells supplied by commercial vendors. Am. J. Physiol. Cell Physiol. 2015, 308, C578–C580. [Google Scholar] [CrossRef] [Green Version]
- Fisher, M.C.; Hawkins, N.J.; Sanglard, D.; Gurr, S.J. Worldwide emergence of resistance to antifungal drugs challenges human health and food security. Science 2018, 360, 739–742. [Google Scholar] [CrossRef] [Green Version]
- Sansone-Parsons, A.; Krishna, G.; Simon, J.; Soni, P.; Kantesaria, B.; Herron, J.; Stoltz, R. Effects of Age, Gender, and Race/Ethnicity on the Pharmacokinetics of Posaconazole in Healthy Volunteers. Antimicrob. Agents Chemother. 2007, 51, 495–502. [Google Scholar] [CrossRef] [Green Version]
- Popp, C.; Ramírez-Zavala, B.; Schwanfelder, S.; Krüger, I.; Morschhäuser, J. Evolution of Fluconazole-Resistant Candida albicans Strains by Drug-Induced Mating Competence and Parasexual Recombination. MBio 2019, 10, e02740-18. [Google Scholar] [CrossRef] [Green Version]
- Campione, E.; Marino, D.; Orlandi, A.; Gaziano, R. Fungistatic activity of all-trans retinoic acid against Aspergillus fumigatus and Candida albicans. Drug Des. Devel. Ther. 2016, 10, 1551. [Google Scholar] [CrossRef] [Green Version]
- Campione, E.; Cosio, T.; Lanna, C.; Mazzilli, S.; Ventura, A.; Dika, E.; Gaziano, R.; Dattola, A.; Candi, E.; Bianchi, L. Predictive role of vitamin A serum concentration in psoriatic patients treated with IL-17 inhibitors to prevent skin and systemic fungal infections. J. Pharmacol. Sci. 2020, 144, 52–56. [Google Scholar] [CrossRef]
- Cosio, T.; Gaziano, R.; Zuccari, G.; Costanza, G.; Grelli, S.; Di Francesco, P.; Bianchi, L.; Campione, E. Retinoids in Fungal Infections: From Bench to Bedside. Pharmaceuticals 2021, 14, 962. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kraševec, N. The Multifaceted Role of Mating Type of the Fungus and Sex of the Host in Studies of Fungal Infections in Humans. J. Fungi 2022, 8, 461. https://doi.org/10.3390/jof8050461
Kraševec N. The Multifaceted Role of Mating Type of the Fungus and Sex of the Host in Studies of Fungal Infections in Humans. Journal of Fungi. 2022; 8(5):461. https://doi.org/10.3390/jof8050461
Chicago/Turabian StyleKraševec, Nada. 2022. "The Multifaceted Role of Mating Type of the Fungus and Sex of the Host in Studies of Fungal Infections in Humans" Journal of Fungi 8, no. 5: 461. https://doi.org/10.3390/jof8050461