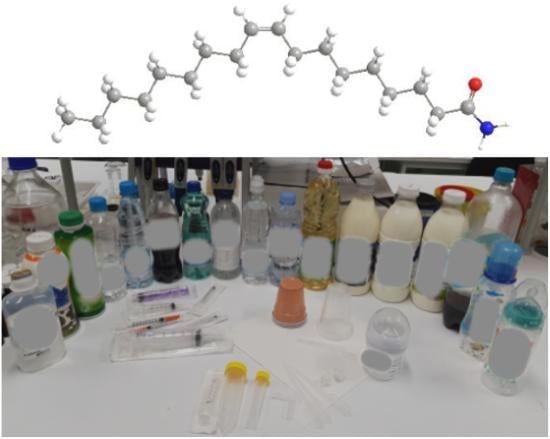
Oleamide, a Bioactive Compound, Unwittingly Introduced into the Human Body through Some Plastic Food/Beverages and Medicine Containers
Abstract
:1. Introduction
2. Materials and Methods
2.1. Chemicals and Materials
2.2. Preparation of Extracts of Medicinal Plastic Materials
2.3. Preparation of Extracts of Baby Bottles and Plastic Food/Beverages Containers
2.4. LC-MS Analysis
2.5. Statistical Analysis
2.6. Identification of the Source of Migrated Oleamide
3. Results and Discussion
3.1. LC-MS Method
3.2. Medicinal Plastic Materials
3.3. Baby Bottles and Plastic Food/Beverages Containers
3.4. Identification of the Source of Migrated Oleamide
3.5. Screening of Other Extractables and Leachables
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jenke, D.; Odufu, A.; Couch, T.; Chacko, M.; Strathmann, S.; Edgcomb, E. Evaluation of the general solution compatibility of polymer materials used in medical devices such as syringes. PDA J. Pharm. Sci. Technol. 2012, 66, 286–306. [Google Scholar] [CrossRef] [PubMed]
- Hahladakis, J.N.; Velis, C.A.; Weber, R.; Iacovidou, E.; Purnell, P. An overview of chemical additives present in plastics: Migration, release, fate and environmental impact during their use, disposal and recycling. J. Hazard. Mater. 2018, 344, 179–199. [Google Scholar] [CrossRef] [PubMed]
- Farajzadeh, M.A.; Ebrahimi, M.; Ranji, A.; Feyz, E.; Bejani, V.; Matin, A.A. HPLC and GC methods for determination of lubricants and their evaluation in analysis of real samples of polyethylene. Microchim. Acta 2005, 153, 73–78. [Google Scholar] [CrossRef]
- Lau, O.W.; Wong, S.K. Contamination in food from packaging material. J. Chromatogr. A 2000, 882, 255–270. [Google Scholar] [CrossRef]
- Jenke, D.R. Extractables and leachables considerations for prefilled syringes. Expert Opin. Drug Deliv. 2014, 11, 1591–1600. [Google Scholar] [CrossRef] [PubMed]
- Kluwe, W.M.; Haseman, J.K.; Huff, J.E. The carcinogenicity of di (2-ethylhexyl) phthalate (dehp) in perspective. J. Toxicol. Environ. Health 1983, 12, 159–169. [Google Scholar] [CrossRef]
- Chen, X.; Xu, S.; Tan, T.; Lee, S.T.; Cheng, S.H.; Lee, F.W.F.; Xu, S.J.L.; Ho, K.C. Toxicity and estrogenic endocrine disrupting activity of phthalates and their mixtures. Int. J. Environ. Res. Public Health 2014, 11, 3156–3168. [Google Scholar] [CrossRef]
- Halden, R.U. Plastics and Health Risks. Annu. Rev. Public Health 2010, 66, 286–306. [Google Scholar] [CrossRef] [Green Version]
- Cooper, I.; Tice, P.A. Migration studies on fatty acid amide slip additives from plastics into food simulants. Food Addit. Contam. 1995, 12, 235–244. [Google Scholar] [CrossRef]
- Simoneau, C.; Van den Eede, L.; Valzacchi, S. Identification and quantification of the migration of chemicals from plastic baby bottles used as substitutes for polycarbonate. Food Addit. Contam. Part A Chem. Anal. Control. Expo. Risk Assess. 2012, 29, 469–480. [Google Scholar] [CrossRef] [Green Version]
- Bisogno, T.; Sepe, N.; De Petrocellis, L.; Mechoulam, R.; Di Marzo, V. The sleep inducing factor oleamide is produced by mouse neuroblastoma cells. Biochem. Biophys. Res. Commun. 1997, 239, 473–479. [Google Scholar] [CrossRef]
- Cravatt, B.F.; Prospero-Garcia, O.; Siuzdak, G.; Gilula, N.B.; Henriksen, S.J.; Boger, D.L.; Lerner, R.A. Chemical characterization of a family of brain lipids that induce sleep. Science 1995, 268, 1506–1509. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rueda-Orozco, P.E.; Montes-Rodriguez, C.J.; Ruiz-Contreras, A.E.; Mendez-Diaz, M.; Prospero-Garcia, O. The effects of anandamide and oleamide on cognition depend on diurnal variations. Brain Res. 2017, 1672, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Mendelson, W.B.; Basile, A.S. The hypnotic actions of the fatty acid amide, oleamide. Neuropsychopharmacology 2001, 25, S36–S39. [Google Scholar] [CrossRef]
- McDonald, G.R.; Hudson, A.L.; Dunn, S.M.J.; You, H.; Baker, G.B.; Whittal, R.M.; Martin, J.W.; Jha, A.; Edmondson, D.E.; Holt, A. Bioactive contaminants leach from disposable laboratory plasticware. Science 2008, 322, 917. [Google Scholar] [CrossRef]
- Langstein, J.; Hofstädter, F.; Schwarz, H. Cis-9,10-octadecenoamide, an endogenous sleep-inducing CNS compound, inhibits lymphocyte proliferation. Res. Immunol. 1996, 147, 389–396. [Google Scholar] [CrossRef]
- Oh, Y.T.; Lee, J.Y.; Lee, J.; Lee, J.H.; Kim, J.E.; Ha, J.; Kang, I. Oleamide suppresses lipopolysaccharide-induced expression of iNOS and COX-2 through inhibition of NF-κB activation in BV2 murine microglial cells. Neurosci. Lett. 2010, 474, 148–153. [Google Scholar] [CrossRef]
- Moon, S.M.; Lee, S.A.; Hong, J.H.; Kim, J.S.; Kim, D.K.; Kim, C.S. Oleamide suppresses inflammatory responses in LPS-induced RAW264.7 murine macrophages and alleviates paw edema in a carrageenan-induced inflammatory rat model. Int. Immunopharmacol. 2018, 56, 179–185. [Google Scholar] [CrossRef]
- Yang, W.S.; Lee, S.R.; Jeong, Y.J.; Park, D.W.; Cho, Y.M.; Joo, H.M.; Kim, I.; Seu, Y.B.; Sohn, E.H.; Kang, S.C. Antiallergic activity of ethanol extracts of Arctium lappa L. undried roots and its active compound, oleamide, in regulating FcϵRI-mediated and MAPK signaling in RBL-2H3 cells. J. Agric. Food Chem. 2016, 64, 3564–3573. [Google Scholar] [CrossRef]
- Dublin City University, Dublin 9 (IE). A Method of Treating Peripheral Inflammatory Disease. European Patent Application No. 15168496.6, 20 May 2015.
- Cani, P.D.; Plovier, H.; Van Hul, M.; Geurts, L.; Delzenne, N.M.; Druart, C.; Everard, A. Endocannabinoids—At the crossroads between the gut microbiota and host metabolism. Nat. Rev. Endocrinol. 2016, 12, 133–143. [Google Scholar] [CrossRef]
- Olivieri, A.; Degenhardt, O.S.; Mcdonald, G.R.; Narang, D.; Paulsen, I.M.; Kozuska, J.L.; Holt, A. On the disruption of biochemical and biological assays by chemicals leaching from disposable laboratory plasticware. Can. J. Physiol. Pharmacol. 2012, 90, 697–703. [Google Scholar] [CrossRef]
- Hiley, C.R.; Hoi, P.M. Oleamide: A fatty acid amide signaling molecule in the cardiovascular system? Cardiovasc. Drug Rev. 2007, 25, 46–60. [Google Scholar] [CrossRef] [PubMed]
- Jug, U.; Naumoska, K.; Metličar, V.; Schink, A.; Makuc, D.; Vovk, I.; Plavec, J.; Lucas, K. Interference of oleamide with analytical and bioassay results. Sci. Rep. 2020, 10, 2163. [Google Scholar] [CrossRef]
- Vera, P.; Canellas, E.; Nerín, C. Identification of non volatile migrant compounds and NIAS in polypropylene films used as food packaging characterized by UPLC-MS/QTOF. Talanta 2018, 188, 750–762. [Google Scholar] [CrossRef] [PubMed]
- Vera, P.; Canellas, E.; Barknowitz, G.; Goshawk, J.; Nerín, C. Ion-mobility quadrupole time-of-flight mass spectrometry: A novel technique applied to migration of nonintentionally added substances from polyethylene films intended for use as food packaging. Anal. Chem. 2019, 91, 12741–12751. [Google Scholar] [CrossRef]
- García Ibarra, V.; Rodríguez Bernaldo de Quirós, A.; Paseiro Losada, P.; Sendón, R. Non-target analysis of intentionally and non intentionally added substances from plastic packaging materials and their migration into food simulants. Food Packag. Shelf Life 2019, 21, 100325. [Google Scholar] [CrossRef]
- Carrero-Carralero, C.; Escobar-Arnanz, J.; Ros, M.; Jiménez-Falcao, S.; Sanz, M.L.; Ramos, L. An untargeted evaluation of the volatile and semi-volatile compounds migrating into food simulants from polypropylene food containers by comprehensive two-dimensional gas chromatography-time-of-flight mass spectrometry. Talanta 2019, 195, 800–806. [Google Scholar] [CrossRef]
- Zimmermann, L.; Dierkes, G.; Ternes, T.A.; Völker, C.; Wagner, M. Benchmarking the in Vitro Toxicity and Chemical Composition of Plastic Consumer Products. Environ. Sci. Technol. 2019, 53, 11467–11477. [Google Scholar] [CrossRef] [Green Version]
- Rajbux, C.; Pereira, J.; Selbourne, M.D.C.; Costa-Pinto, A.R.; Poças, F. Assessment of baby Bibs. GC-MS screening, migration into saliva and insight of toxicity with QSAR tools. Food Control 2020, 109, 106951. [Google Scholar] [CrossRef]
- Kuki, Á.; Zelei, G.; Nagy, L.; Nagy, T.; Zsuga, M.; Kéki, S. Rapid mapping of various chemicals in personal care and healthcare products by direct analysis in real time mass spectrometry. Talanta 2019, 192, 241–247. [Google Scholar] [CrossRef]
- Commission Regulation (EU) No 10/2011 of 14 January 2011 on Plastic Materials and Articles Intended to Come into Contact with Food Text with EEA Relevance. Available online: https://publications.europa.eu/sl/publication-detail/-/publication/84665a0a-f9e5-4eae-aac5-af4fd4c8ac94/language-en (accessed on 15 April 2019).
- Divito, E.B.; Davic, A.P.; Johnson, M.E.; Cascio, M. Electrospray ionization and collision induced dissociation mass spectrometry of primary fatty acid amides. Anal. Chem. 2012, 84, 2388–2394. [Google Scholar] [CrossRef] [PubMed]
- Crozier Willi, G.; Berger, A.; Di Marzo, V.; Bisogno, T.; De Petrocellis, L.; Fride, E.; Mechoulam, R. Lipids in neural function: Modulation of behavior by oral administration of endocannabinoids found in foods. Nestle Nutr. Workshop Ser. Clin. Perform. Programme 2001, 5, 169–187. [Google Scholar] [PubMed] [Green Version]
- Bradley, E.; Coulier, L. An Investigation into the Reaction and Breakdown Products from Starting Substances Used to Produce Food Contact Plastics; Report FD 07/01; Central Science Laboratory: Sand Hutton, York, UK, 2007. [Google Scholar]
- Bach, C.; Dauchy, X.; Chagnon, M.; Etienne, S.; Bach, C.; Dauchy, X.; Chagnon, M.; Etienne, S. Chemical migration in drinking water stored in polyethylene terephthalate (PET) bottles: A source of controversy. Water Res. Elsevier 2012, 46, 571–583. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shi, Y.; Liu, H.H.; Rule, M. Packaged Potable Liquid with UV Absorber for Reduced Off-Taste from Closure and Method. U.S. Patent Application Publication No.: US 2004/0185196 A1, 21 March 2003. [Google Scholar]
- Gorji, S.; Biparva, P.; Bahram, M.; Nematzadeh, G. Development of magnetic solid phase microextraction method for determination of the endocrine disrupting chemicals leached from reused plastic bottles. Talanta 2019, 194, 859–869. [Google Scholar] [CrossRef]
- Buiarelli, F. HPLC and GC-MS detection of compounds released to mineral waters stored inplastic bottles of PET and PVC. Ann. Di Chim. 1993, 83, 93–104. [Google Scholar]
- Cooper, I.; Lord, T.; Tice, P.A. Hydrolysis studies on oleamide in simulated gastrointestinal fluids. Food Addit. Contam 1995, 12, 769–777. [Google Scholar] [CrossRef]
- Osmundsen, P.E. Contact urticaria from nickel and plastic additives. Contact Dermat. 1980, 6, 452–454. [Google Scholar] [CrossRef]
- Aalto-Korte, K.; Pesonen, M.; Kuuliala, O.; Suuronen, K. Contact allergy from metalworking fluid traced to tall oil fatty acids monoethanolamide. Contact Dermat. 2013, 69, 316–317. [Google Scholar] [CrossRef]
- Barlow, S. Threshold of toxicological concern (TTC). In ILSI Eur. Concise Monogr. Ser.; ILSI Press: Washington DC, USA, 2005; ISBN 1-57881-188-0. [Google Scholar]
- Kroes, R.; Renwick, A.G.; Cheeseman, M.; Kleiner, J.; Mangelsdorf, I.; Piersma, A.; Schilter, B.; Schlatter, J.; van Schothorst, F.; Vos, J.G.; et al. Structure-based thresholds of toxicological concern (TTC): Guidance for application to substances present at low levels in the diet. Food Chem. Toxicol. 2004, 42, 65–83. [Google Scholar] [CrossRef]
- Draft Screening Assessment Fatty Amides Group, Environment and Climate Change Canada, Health Canada. 2018. Available online: https://www.canada.ca/en/environment-climate-change/services/evaluating-existing-substances/screening-assessment-fatty-amides.html (accessed on 9 April 2020).
- Bengström, L. Chemical Identification of Contaminants in Paper and Board Food Contact Materials. Ph.D. Thesis, Technical University of Lyngby, Denmark, Denmark, 2014. [Google Scholar]
- ESI Common Background Ions, UWPR. Advancing Proteomics. Available online: http://www.proteomicsresource.washington.edu/protocols05/esi_background_ions.php (accessed on 15 April 2019).
- Common LC/MS Contaminants, Agilent Technologies, September 2003. Available online: https://view.officeapps.live.com/op/view.aspx?src=https%3A%2F%2Fwww.cigs.unimo.it%2Fcigsdownloads%2Flabs%2Flcmsit%2Fcontaminants%2520ion%2520trap.doc (accessed on 9 April 2020).
- Keller, B.O.; Sui, J.; Young, A.B.; Whittal, R.M. Interferences and contaminants encountered in modern mass spectrometry. Anal. Chim. Acta 2008, 627, 71–81. [Google Scholar] [CrossRef]
- BACKGROUND ION LIST, Rev. A, Waters. Available online: https://www.waters.com/webassets/cms/support/docs/bkgrnd_ion_mstr_list.pdf (accessed on 15 April 2019).
- Bertin, M.J.; Zimba, P.V.; Beauchesne, K.R.; Huncik, K.M.; Moeller, P.D.R. Identification of toxic fatty acid amides isolated from the harmful alga Prymnesium parvum carter. Harmful Algae 2012, 20, 111–116. [Google Scholar] [CrossRef]
- Beißmann, S.; Stiftinger, M.; Grabmayer, K.; Wallner, G.; Nitsche, D.; Buchberger, W. Monitoring the degradation of stabilization systems in polypropylene during accelerated aging tests by liquid chromatography combined with atmospheric pressure chemical ionization mass spectrometry. Polym. Degrad. Stab. 2013, 98, 1655–1661. [Google Scholar] [CrossRef]

| Material Tested with LC-MS Method | Type of a Polymer | Extraction Media/Type of Simulant | Contact Conditions | Pre-treatment before Analysis | Presence of Oleamide Peak in SIM (m/z 282) | Concentration of Oleamide in Extraction Media (ng mL−1) | Estimated Intake of Oleamide (µg) Per Volume (mL) of the Tested Material |
|---|---|---|---|---|---|---|---|
| Medicinal plastic material | |||||||
| Intravenous infusion bottle A | LDPE | S (EtOH10) | 10 days, 60 °C | conc. | + | 17 ± 1 *** | 4/250 |
| Syringe 5mL B | PP + PE | MeOH | non conc. | + | 7351 ± 1963 * | / | |
| Syringe 5mL B | PP + PE | S (H2O) | conc. | + | 12 ± 3 ** | 0.06/5 | |
| Syringe 5mL C | PP + PE | MeOH | non conc. | - | <LOQ | / | |
| Syringe 5mL C | PP + PE | MeOH | conc. | + | <LOQ | / | |
| Syringe 5mL C | PP + PE | S (H2O) | conc. | - | <LOQ | / | |
| Insulin syringe 1 mL D | PP | MeOH | non conc. | + | 21,984 ± 1155 *** | / | |
| Insulin syringe 1 mL D | PP | S (H2O) | conc. | + | 152 ± 8 *** | 0.15/1 | |
| Insulin syringe 1 mL B | LDPE | MeOH | non conc. | - | <LOQ | / | |
| Insulin syringe 1 mL B | LDPE | MeOH | conc. | - | <LOQ | / | |
| Insulin syringe 1 mL B | LDPE | S (H2O) | conc. | - | <LOQ | / | |
| Enteral syringe E | PP | MeOH | non conc. | - | <LOQ | / | |
| Enteral syringe E | PP | MeOH | conc. | + | <LOQ | / | |
| Enteral syringe E | PP | FS (EtOH50) | conc. | - | <LOQ | / | |
| Baby bottles | |||||||
| Baby bottle F | PP | FS (EtOH50) | 2 h, 40 °C | conc. | + | 23 ± 3 ** | 3/125 |
| Baby bottle G | PP | FS (EtOH50) | 2 h, 40 °C | conc. | + | 12 ± 2 ** | 3/250 |
| Baby bottle H | PP | FS (EtOH50) | 2 h, 40 °C | conc. | + | 20 ± 2 ** | 6/300 |
| Dummy F | silicon | MeOH | conc. | + | 33 ± 8 ** | / | |
| Dummy G | silicon | MeOH | conc. | + | 30 ± 4 ** | / | |
| Dummy H | silicon | MeOH | conc. | + | 39 ± 9 ** | / | |
| Plastic food containers | |||||||
| Carbonated soft drink I | PET | FS (AC3) | 10 days, 60 °C | conc. | + | 15 ± 3 ** | 8/500 |
| Carbonated soft drink J | PET | FS (AC3) | 10 days, 60 °C | conc. | + | 6 ± 1 ** | 9/1500 |
| Vitamin water K | PET | FS (AC3) | 10 days, 60 °C | conc. | + | 15 ± 3 ** | 8/500 |
| Milk (3.5% fat) L | PET | FS (EtOH50) | 10 days, 20 °C | conc. | + | 3 ± 2 * | 3/1000 |
| Milk (3.5% fat) M | PET | FS (EtOH50) | 10 days, 20 °C | conc. | + | 9 ± 5 * | 9/1000 |
| Milk (1.5% fat) N | PET | FS (EtOH50) | 10 days, 20 °C | conc. | + | 8 ± 3 * | 8/1000 |
| Liquid yogurt (4% fat) O | PET | FS (EtOH50) | 10 days, 20 °C | conc. | + | 17 ± 3 ** | 9/500 |
| Liquid yogurt (1.3% fat) P | PET | FS (EtOH50) | 10 days, 20 °C | conc. | + | 17 ± 2 ** | 8/500 |
| Oil N | PET | FS (oil = RS) | 10 days, 60 °C | LLE + conc. | + | 238 ± 21 ** | 238/1000 |
| Milk (3.5% fat) M | PET | RS (milk) | LLE + conc. | + | 293 ± 47 * | 293/1000 | |
| Oil N | PET | RS (oil) | LLE + conc. | + | 217 ± 9 *** | 217/1000 | |
| Water Q | PET | RS (water) | 10 days, 60 °C | conc. | + | 16 ± 2 ** | 8/500 |
| Water R | PET | RS (water) | 10 days, 60 °C | conc. | + | 11 ± 1 *** | 6/500 |
| Water S | PET | RS (water) | 10 days, 60 °C | conc. | + | 12 ± 3 ** | 6/500 |
| Water G | PET | RS (water) | 10 days, 60 °C | conc. | + | 12 ± 2 ** | 6/500 |
| Water T | PET | RS (water) | 10 days, 60 °C | conc. | + | 18 ± 4 ** | 9/500 |
| Water N | PET | RS (water) | 10 days, 60 °C | conc. | + | 14 ± 2 ** | 7/500 |
| Material Tested | Tested Parts | |
|---|---|---|
| barrel | plunger | |
| Syringe 5 mL B | + | + |
| Insulin syringe 1 mL D | + | + |
| container | dummy | |
| Baby bottle and dummy F | + | + |
| Baby bottle and dummy G | + | + |
| Baby bottle and dummy H | + | + |
| container | closure | |
| Intravenous infusion bottle A | + | + |
| Carbonated soft drink I | + | + |
| Carbonated soft drink J | + | + |
| Vitamin water K | + | + |
| Milk (3.5% fat) L | + | + |
| Milk (3.5% fat) M | + | + |
| Milk (1.5% fat) N | + | + |
| Liquid yogurt (4% fat) O | + | + |
| Liquid yogurt (1.3% fat) P | + | + |
| Oil N | + | + |
| Water Q | + | + |
| Water R | + | + |
| Water S | + | + |
| Water G | + | + |
| Water T | + | + |
| Water N | + | + |
| m/z (ESI+) | Tentative Identification | tR (min) | Material | Reference |
|---|---|---|---|---|
| 228 | N-butyl-p-toluenesulphonamide; unknown (present in oleamide standard); myristamide | 8.44 | Insulin syringe (1 mL), plastic syringe (5 mL) | [33,35,46] |
| 242 | Tetrabutylammonium cation | 11.03, 12.16 | Plastic syringe (5 mL) | [47] |
| 245 | Oxotris(propan-2-olato)vanadium; 2,2’-dihydroxy-4-methoxybenzophenone; 1,1’-azobis(cyclohexanecarbonitrile); 2,2’-dimethoxy-4,4’-benzidine; | 8.45 | Insulin syringe (1 mL), plastic syringe (5 mL) | [46] |
| 250 | Triallyl (iso)cyanurate | 9.04 | Dummy | [46] |
| 254 | Unsaturated amine (present in oleamide standard) | 10.37 | Insulin syringe (1 mL), plastic syringe (5 mL) | [35] |
| 256 | C14 Unsaturated mono alcohol derivative (present in oleamide standard); palmitamide | 18.41 | Insulin syringe (1 mL), plastic syringe (5 mL) | [33,35] |
| 268 | ? | 14.89 | Insulin syringe (1 mL), plastic syringe (5 mL) | [48] |
| 273 | Tetrapropylene glycol [M+Na]+; monomethoxytrityl cation | 18.41 | Insulin syringe (1 mL), plastic syringe (5 mL) | [47,49,50] |
| 278 | 2-Ethylhexyl-4-(dimethyl amino) benzoate; ethyl 2-cyano-3,3-diphenylacrylate | 8.97 | Plastic syringe (5 mL) | [46] |
| 280 | Unknown (present in oleamide standard) - oxidation product? | 13.49, 14.89 | Insulin syringe (1 mL), plastic syringe (5 mL) | [35] |
| 282 | Trans-oleamide (elaidamide) | 23.77 | Insulin syringe (1 mL), plastic syringe (5 mL) | [51] |
| 284 | Oleamide contaminant; stearamide; | 6.05, 21.07 | Plastic syringe (5 mL) | [33,35,47,48] |
| 284 | Oleamide contaminant; stearamide; | 6.05 | Food container | [33,35,47,48] |
| 301 | Oleoyl chloride; dibutylphthalate [M+Na]+; sodium (C10-C18) alkyl sulfonate; (nonylphenyl)phosphate | 6.05, 21.07 | Plastic syringe (5 mL) | [35,47,49,51] |
| 310 | ? | 11.03 | Plastic syringe (5 mL) | |
| 314 | Ethyl stearate; styrene trimer | 5.54 | Food container, baby bottle, dummy | [35] |
| 331 | Pentadecyl sodium sulfate; pentapropylene glycol [M+Na]+; dicyclohexyl phthalate | 23.19 | Baby bottle, food container | [35,47,49] |
| 341 | Glycerol monostearate [M+H-H2O]+; unknown | 18.54 | Baby bottle | [35] |
| 348 | ? | 23.19 | Baby bottle | |
| 359 | Heptadecyl sodium sulfate | 18.54 | Baby bottle | [35] |
| 362 | 2-Ethylhexyl 2-cyano-3,3-diphenylacrylate; 2-(4-dodecylphenyl)indole; didecyldimethylammonium chloride | 9.04 | Dummy | [46] |
| 368 | N,N,N-Trimethyldocosan-1-aminium cation | 8.97, 10.43 | Plastic syringe (5 mL) | [47,49] |
| 369 | 2,2’-(1,4-phenylene) bis[4H-3,1-benzoxazin-4-one]; N-[2-[(2-hydroxyethyl)amino]ethyl]oleamide; 2,2’-methylene bis(4-ethyl-6-tert-butylphenol); lignoceric acid; 2-ethylhexyl palmitate | 23.19 | Baby bottle | [46] |
| 371 | Decamethylcyclopentasiloxane; pentasiloxane; octaethylene glycol; dioctyl adipate; bis(2-ethylhexyl) adipate | 6.40 | Food container, baby bottle, dummy | [47,48,49,51] |
| 376 | 1,3,5-Tris (2,2-dimethylpropionylamino)-benzene; sodium 3-[(4-anilinophenyl)diazenyl]benzenesulfonate (Acid Yellow 36) | 18.54 | Baby bottle | [46] |
| 379 | α-Cyano-4-hydroxycinnamic acid [M2+H]+ | 9.04 | Dummy | [47,49] |
| 385 | Bisphenol F bis(2-chloro-1-propanol) ether | 6.31 | Food container, baby bottle, dummy | [46] |
| 397 | ? | 18.54 | Baby bottle | [47,49] |
| 399 | Setoglaucine (Basic Blue 1); tris-(2-butoxyethyl) phosphate; decyl octyl adipate | 4.25, 13.29 | Dummy | [46] |
| 403 | Acetyltributyl citrate; glyceryl monooleate [M+H+CH2O2]+; unknown | 5.54 | Food container, baby bottle, dummy | [34] |
| 426 | 2-(4,6-Diphenyl-1,3,5-triazin-2-yl)-5-(hexyloxy)phenol | 20.93, 23.59 | Infusion bottle, food container, baby bottle, dummy | [46] |
| 431 | 2,5-Bis(5’-tert-butylbenzoxazol-2-yl)thiophene | 12.03 | Dummy | [35,48] |
| 455 | ? | 8.45 | Plastic syringe (5 mL) | [47,49] |
| 456 | ? | 20.93–23.00 | Infusion bottle, food container, baby bottle, dummy | |
| 463 | Septapropylene glycol [M+K]+; | 18.50 | Dummy | [49] |
| 480 | ? | 18.50 | Dummy | |
| 485 | ? | 2.19 | Food container | [47,49] |
| 485 | ? | 2.19, 10.76 | Baby bottle | [47,49] |
| 486 | ? | 2.26, 4.65 | Infusion bottle | |
| 491 | Bisphenol A diglycidyl ether; derivative | 18.50, 21.60 | Dummy | [46] |
| 502 | ? | 9.19 | Baby bottle | |
| 511 | 1-Piperidinyloxy, 4,4’-[1,10-dioxo-1,10-decanediyl)bis(oxy)]bis[2,2,6,6-tetramethyl] | 17.80 | Plastic syringe (5 mL) | [46] |
| 563 | 4,4’-Bis(2-sulphostyryl)biphenyl, disodium salt | 21.00 | Insulin syringe (1 mL), plastic syringe (5 mL) | [46] |
| 567 | Irganox 1330 fragment (2,6-di-tert-butylphenol split off) | 4.25 | Dummy | [52] |
| 740 | ? | 4.39 | Infusion bottle | |
| 953 | ? | 7.91 | Infusion bottle | [47] |
| 955 | ? | 4.45, 7.91 | Infusion bottle |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Naumoska, K.; Jug, U.; Metličar, V.; Vovk, I. Oleamide, a Bioactive Compound, Unwittingly Introduced into the Human Body through Some Plastic Food/Beverages and Medicine Containers. Foods 2020, 9, 549. https://doi.org/10.3390/foods9050549
Naumoska K, Jug U, Metličar V, Vovk I. Oleamide, a Bioactive Compound, Unwittingly Introduced into the Human Body through Some Plastic Food/Beverages and Medicine Containers. Foods. 2020; 9(5):549. https://doi.org/10.3390/foods9050549
Chicago/Turabian StyleNaumoska, Katerina, Urška Jug, Valentina Metličar, and Irena Vovk. 2020. "Oleamide, a Bioactive Compound, Unwittingly Introduced into the Human Body through Some Plastic Food/Beverages and Medicine Containers" Foods 9, no. 5: 549. https://doi.org/10.3390/foods9050549
APA StyleNaumoska, K., Jug, U., Metličar, V., & Vovk, I. (2020). Oleamide, a Bioactive Compound, Unwittingly Introduced into the Human Body through Some Plastic Food/Beverages and Medicine Containers. Foods, 9(5), 549. https://doi.org/10.3390/foods9050549